AI-powered MRI tool to improve prostate cancer treatment
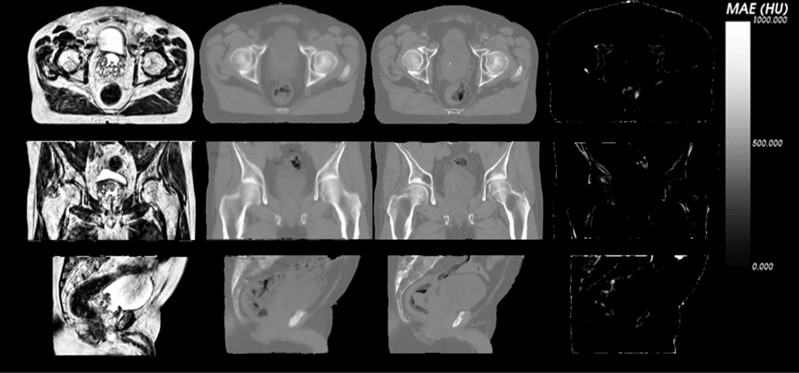
CSIRO has developed software to better guide radiation therapy treatment. The software has been designed to reduce damage to surrounding, normal, tissue. From left to right: sample patient MRI, CSIRO generated CT, actual planning CT, and the difference.
MRI-based planning: the next generation for radiation therapy treatment.
The challenge
Radiation therapy is an effective form of treatment for many cancers. However, radiation is damaging to normal tissues.
Image-guided radiation therapy aims to solve this by targeting only the cancerous tissues.
Modern image-guided external beam radiation therapy relies on computed tomography (CT) scans. These 3D scans are geometrically accurate and provide information needed to predict radiation absorption and scattering during treatment delivery.
However, CT scanning is poor at identifying the boundaries and location of soft tissue organs. In prostate cancer treatment, this uncertainty can cause damage to normal tissues such as the bladder and rectum. This can lead to rectal bleeding, incontinence, and erectile problems.
On the other hand, magnetic resonance imaging (MRI) is exceptionally good at identifying soft tissue boundaries. This is used by many centres – a pre-treatment prostate MRI is mapped across to a CT scan. The problem with this solution is twofold: it requires two scanning sessions, and the registration can lead to additional errors (up to 5mm).
Our response
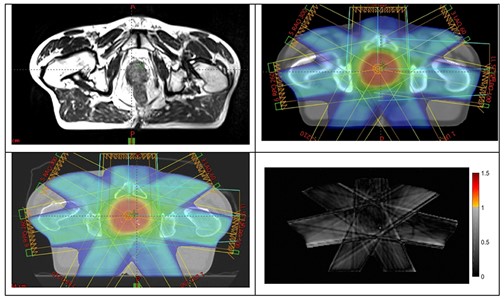
In collaboration with the Calvary Mater Newcastle Hospital’s radiation oncology department, we’ve developed software that integrates with existing radiation oncology workflows and automatically generates CT information and organ boundaries from standard MRI scans.
This software is available on a standalone PC, which can be situated in the MRI console room, or as a cloud application.
The software has been validated in two retrospective clinical trials and a multi-centre prospective clinical trial. The trials demonstrating no significant difference in delivered radiation dose between the MRI-only and CT plans.
Benefits
Our clinically validated software:
- is DICOM-RT based and integrates with existing treatment planning software (such as Varian Eclipse) and existing MRI software
- automatically identifies organs of interest and stores these as DICOM-RT structures for treatment planning
- generates highly accurate CT information from MRI.
By February 2020 over 65 men had received MRI-only prostate cancer treatment using this CSIRO software.
The use of MRI-only treatment planning should result in more accurate treatment with decreased toxicity to healthy tissues. The software should also reduce healthcare costs.
The other major advantage is that MRI-based planning enables the accurate integration of functional information from MRI.
The Australian e-Health Research Centre (AEHRC) is CSIRO's digital health research program and a joint venture between CSIRO and the Queensland Government. The AEHRC works with state and federal health agencies, clinical research groups and health businesses around Australia.
